CanCOLD launches its 4th in-site assessment

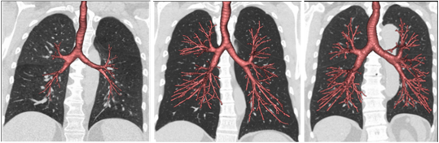
In winter 2022, the CanCOLD study launched visit 4, marking over 10 years of assessments since the baseline study (visit 1) in 2009. At each data collection wave, trained CanCOLD research staff collect a deep pool of information that can be queried to address research questions related to COPD and respiratory health. As with visit 1, this fourth in-site assessment includes a range of health and risk factor questionnaires, blood draws, spirometry tests, pulmonary function tests, cardiopulmonary exercise tests, and multidetector computerized tomography scans (CT Scans). With its rich data collection and over 10 years of follow-up time, this important visit will provide vital data to help us enhance our understanding of lung health in Canada.
CanCOLD visit 4 follows three data collection waves that were completed between 2009 and 2019: baseline assessment occurred between 2009 to 2015, the first follow-up assessment (CanCOLD visit 2) was conducted approximately 18 months after baseline visit (2011 to 2015), and at 3 years post-baseline (2013 to 2019), CanCOLD completed visit 3.
Continuous communication with CanCOLD subjects during and between visits has allowed the study to keep participants engaged and has allowed the project to successfully maintain longitudinal follow-up throughout the years. Currently, all 9 data collection sites are actively contacting participants to collect visit 4 data. By August 2023, close to 100 participants have already completed this fourth assessment site visit, which we expect to unfold until the end of 2024. A decade on, CanCOLD participants are proud to continue to contribute to the scientific knowledge of COPD for the benefit of COPD patient populations and society at large.